Introduction
Heparin-induced thrombocytopenia (HIT) occurs in approximately 0.5-1.0% of patients treated with unfractionated heparin, though true incidence is hard to quantify due to difficulties in recognition and diagnosis. The mainstay of treatment is the initiation of non-heparin anticoagulants until platelet recovery and for one to three months thereafter. There is no available model to predict platelet recovery. A predictive model may help identify (1) patients who are improving even if not reflected in platelet count, particularly in refractory cases; and (2) those who may require adjunctive therapies for treatment.
It has been previously proposed that in a distinct subset of HIT, termed “autoimmune HIT,” the fibrinogen and d-dimer may be helpful markers to assess treatment response. Anecdotally, in complex HIT cases at our institution, we have observed improvements in fibrinogen and d-dimer preceding the resolution of thrombocytopenia. In this study, our aim was to establish a correlation between the fibrinogen, d-dimer, and the platelet count. Fibrinogen and d-dimer assay accessibility make them alluring for widespread use, if informative. We hypothesized that the fibrinogen and d-dimer trends would correlate with improvements in platelets.
Methods
This study design was reviewed and approved by the Vanderbilt University Medical Center (VUMC) Institutional Review Board.
All inpatients admitted to VUMC between August 2022 and March 2023 with a positive HIT immunoassay (ELISA) were identified. Venous blood aliquots in sodium citrate used for anticoagulation management were collected daily. Patients with confirmed HIT based on a positive serotonin release assay were included in the analysis. Samples were collected until resolution of HIT, discharge, and/or death. Fibrinogen and d-dimer were measured on stored samples and compared to the daily platelet counts for each patient.
Statistical Analysis
To determine how baseline platelet count, time, fibrinogen and d-dimer relate to longitudinal measurements of platelet counts (assessed between 1- and 22-days post-baseline) we used a generalized least squares model with an AR1 within-patient correlation pattern, determined using AIC and variograms assessing fit with the data.
Results
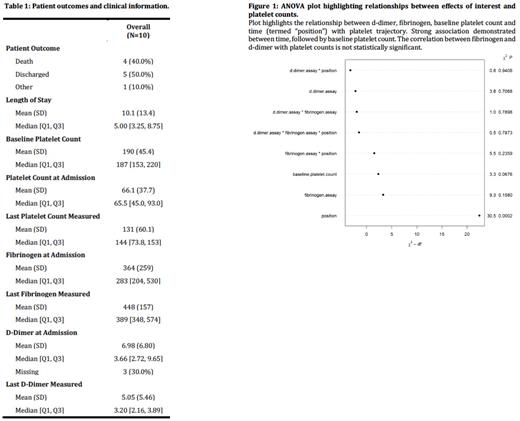
In total, samples from 10 patients with HIT were collected. Baseline characteristics are presented in Table 1. Longitudinal regression analysis presented in the ANOVA plot in Figure 1 suggested that d-dimer ( X2 3.72, p=0.71) and fibrinogen ( X2 9.29, p=0.16) had no statistically significant correlation with platelet recovery, and the only strong variable was time ( X2 30.46, p=0.0002), indicating non-flat trajectories. Baseline platelet count showed signal for positive effect ( X2 3.34, p=0.07). Other effects were assessed, but not significant.
Discussion
The results of our exploratory laboratory correlation study suggest that fibrinogen and d-dimer values were not reliably correlated with platelet counts in patients with HIT, despite anecdotal experience suggesting benefit in monitoring fibrinogen and d-dimer in difficult HIT cases. The best correlation and strongest association with the improvement in platelet counts was time.
Our study has several limitations. First is our small patient sample size. In addition, 4 patients (40%) died due to unrelated complications, therefore limiting the number of data points available for interpretation. Lastly, mean and median fibrinogen values are within the normal range in our data set; d-dimer mean and median are only mildly abnormal. Future prospective studies should be considered to further explore the relationship between fibrinogen and d-dimer with platelet trajectory when markedly abnormal at time of HIT diagnosis, as we have observed in severe HIT cases.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal